Understanding Why Veins Suddenly Become Visible
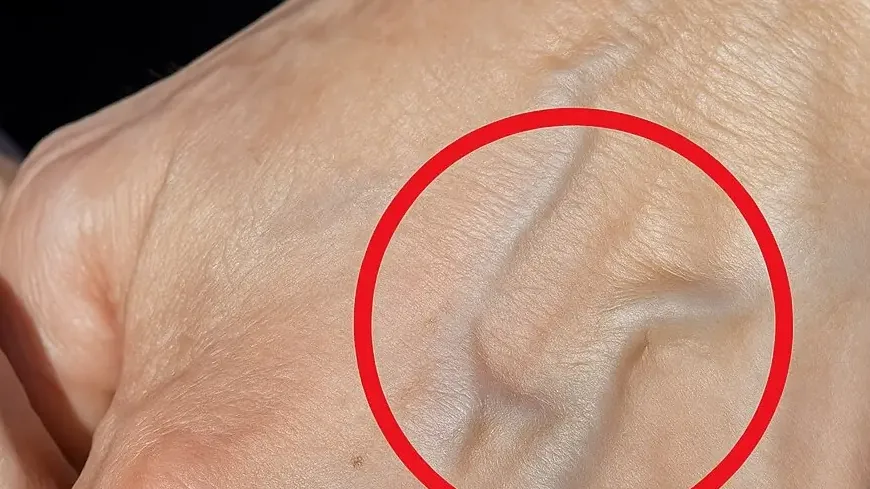
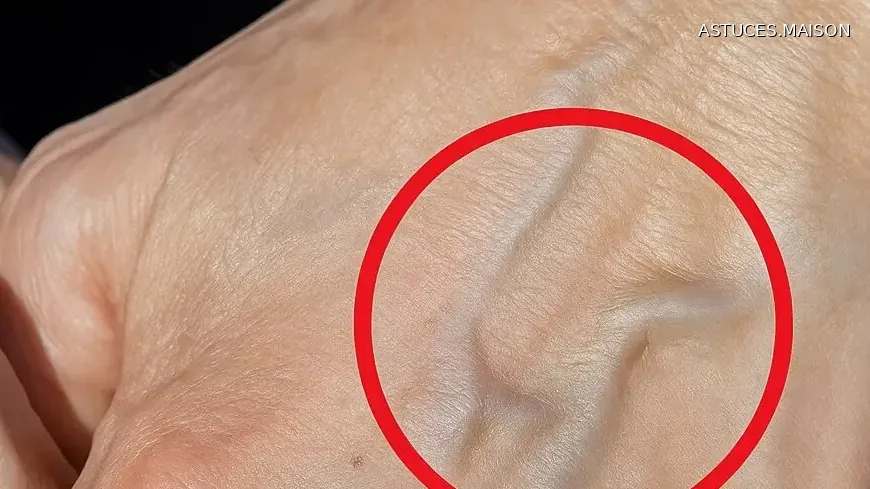
When veins appear seemingly overnight, it’s natural to wonder what’s happening beneath your skin. The truth is, visible veins are often the result of blood pooling in weakened or damaged veins rather than flowing smoothly back to the heart as intended.
Several common factors contribute to this phenomenon. Excessive exercise can temporarily cause veins to bulge as blood flow increases. Aging naturally weakens vein walls and valves, making vessels more prone to expansion. Hot temperatures cause blood vessels to dilate, while tight clothing can restrict proper circulation.
Your genetics also play a significant role—if family members have prominent veins, you’re more likely to develop them too. Sun exposure weakens skin and vein structure over time, and carrying extra weight increases pressure on your circulatory system.
This pooling effect often results in varicose veins, those swollen, twisted veins that typically appear on the legs but can also show up on the arms. While this might sound alarming, it’s important to understand that visible veins are frequently just a cosmetic concern or temporary response to environmental factors.
The key distinction lies in recognizing when these changes represent normal bodily adaptations versus potential medical issues. Most cases of sudden vein visibility have straightforward explanations rooted in lifestyle, age, or genetic predisposition. However, certain accompanying symptoms can signal when these vascular changes deserve closer medical attention.

Medical Conditions Behind Prominent Veins
When visible veins signal more than cosmetic concerns, several medical conditions may be at play. Understanding these conditions helps distinguish between minor issues and situations requiring prompt attention.
Phlebitis represents one of the more common culprits—an inflammation of the veins that creates tenderness and swelling. This condition typically affects surface veins and, while uncomfortable, usually responds well to treatment when caught early.
Varicose veins extend beyond simple visibility concerns. These enlarged, twisted vessels often bring discomfort, aching, or a heavy sensation in affected limbs. Unlike temporary bulging from exercise or heat, varicose veins persist and may worsen without intervention.
Deep vein thrombosis (DVT) demands immediate medical attention as the most serious condition on this spectrum. DVT involves blood clots forming in deep veins, typically in the legs, creating a genuine health emergency. These clots can break loose and travel to the lungs, causing life-threatening complications.
Less commonly, unusual vein patterns appearing on the chest or abdomen may indicate underlying issues affecting internal organs, particularly the liver. While rare, these presentations warrant professional evaluation, especially when accompanied by other systemic symptoms.
Each condition presents distinct characteristics, yet they share the common thread of altered blood flow patterns. The severity ranges from manageable inflammation to emergency situations requiring immediate intervention. Recognizing these differences becomes crucial when visible veins transition from aesthetic concerns to potential health indicators demanding professional assessment.
Warning Signs That Require Attention
Recognizing when visible veins cross the line from normal to concerning requires attention to specific warning signals that your body may send. These indicators help distinguish between harmless changes and situations demanding medical evaluation.
Swelling or pain in the limbs represents the most common red flag accompanying problematic veins. Unlike the temporary discomfort from exercise or prolonged standing, persistent pain or unexplained swelling suggests underlying circulation issues that need professional assessment.
Skin changes around visible veins provide another crucial warning sign. Discoloration—whether darkening, redness, or unusual color variations—often indicates compromised blood flow or inflammation. These changes typically don’t resolve on their own and may worsen without appropriate intervention.
Warmth or redness over affected areas signals active inflammation or infection within the vein system. This combination frequently accompanies more serious conditions like phlebitis or DVT, making prompt medical consultation essential for proper diagnosis and treatment.
Perhaps most concerning are unusual vein patterns appearing suddenly on the chest or abdomen. Unlike the common leg vein issues, these presentations may indicate deeper systemic problems affecting internal organs. The unexpected appearance of prominent veins in these areas warrants immediate professional evaluation.
Skin texture changes around veins—including thickening, scaling, or unusual sensitivity—complete the warning sign spectrum. These alterations often develop gradually but represent clear indicators that the underlying vein issues require medical attention rather than simple monitoring.

When Professional Medical Advice Is Necessary
Understanding these warning signs naturally leads to the question of when professional medical consultation becomes advisable. The decision to seek healthcare guidance doesn’t always require emergency-level symptoms—sometimes prevention and peace of mind justify the conversation.
Veins becoming visible without clear reason represents the primary indication for medical evaluation. When prominent veins appear suddenly without obvious triggers like exercise, heat, or weight changes, professional assessment can identify underlying causes that might otherwise go unnoticed.
Experiencing pain, cramping, or swelling alongside visible veins shifts the situation from observation to action. These symptoms often indicate circulation problems that benefit from early intervention rather than prolonged waiting to see if they resolve independently.
Changes in skin color or texture around veins—as discussed with the warning signs—warrant professional evaluation regardless of their severity. Even subtle alterations may signal developing conditions that respond better to early treatment than delayed intervention.
Perhaps most importantly, seeking peace of mind through professional consultation represents a perfectly valid reason for medical discussion. Healthcare providers understand that vein changes can cause anxiety, and addressing concerns early often prevents unnecessary worry while ensuring proper monitoring.
Most visible veins result from normal body adaptations to activity, temperature, or aging changes. However, when anything seems unusual or uncertain, discussing these observations with a healthcare provider supports proactive health management. Understanding your body’s signals remains key to maintaining optimal health and catching potential issues before they develop into more serious concerns.
Continue Reading →