Understanding The Science Behind Bulging Veins
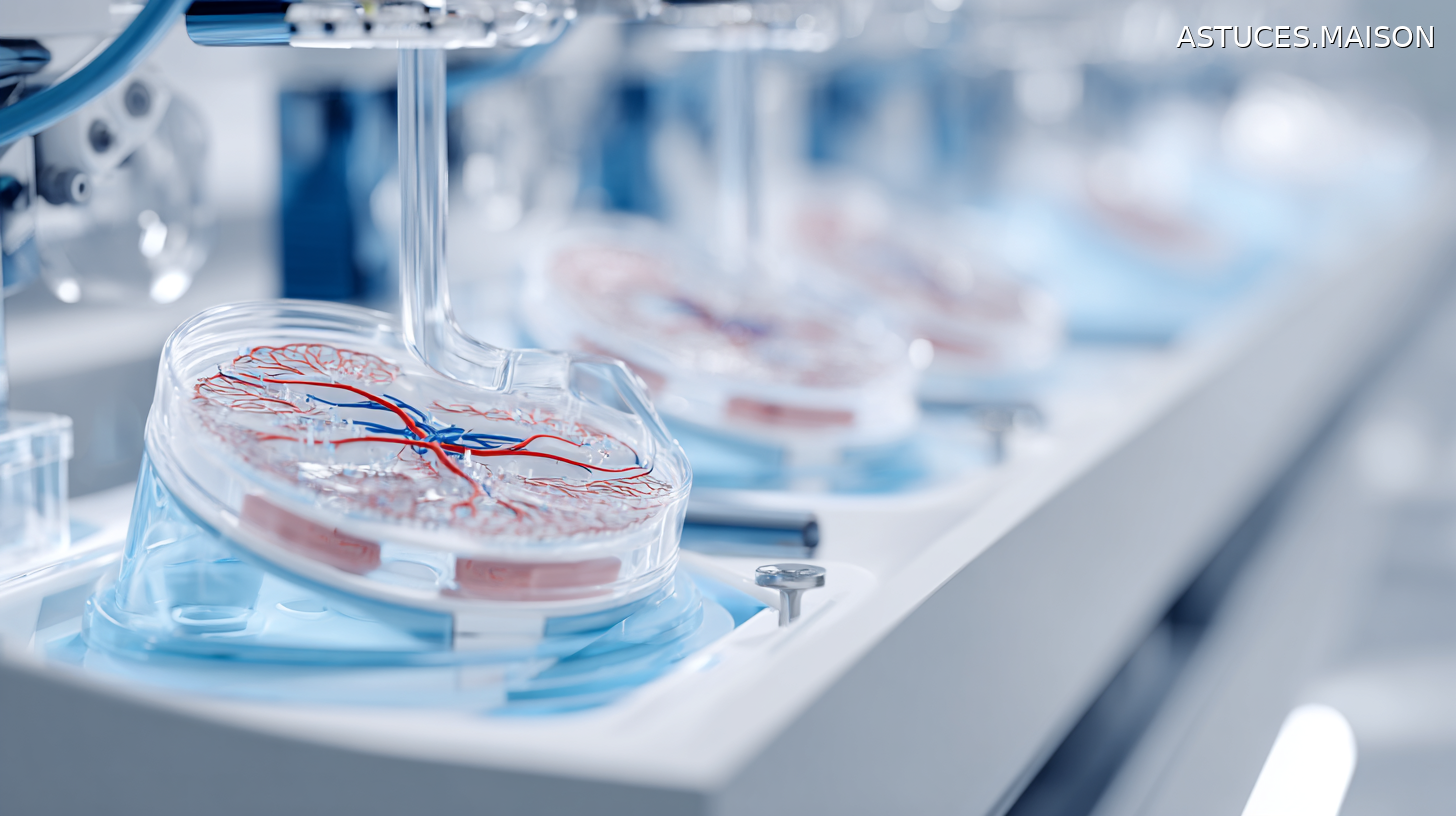
The sudden appearance of prominent veins often stems from fundamental changes in how blood circulates through your body. Veins serve as the circulatory system’s return pathway, transporting deoxygenated blood from tissues back to the heart. This complex network relies on one-way valves strategically positioned throughout each vein to prevent blood from flowing backward due to gravity.
When these crucial valves malfunction or weaken, blood begins pooling in the affected vessels instead of flowing efficiently toward the heart. This accumulation creates internal pressure that forces vein walls to stretch and expand, causing them to bulge outward beneath the skin surface. The process transforms normally flat veins into the raised, twisted formations that become visibly prominent.
The circulatory system distinguishes between different types of visible veins based on their size and location. Spider veins develop in small blood vessels and capillaries, creating thin, web-like patterns that display red or blue coloration while remaining flat against the skin. These smaller vessels rarely bulge above skin level and typically require no medical intervention.
Varicose veins represent the larger, more problematic counterpart that develops when major veins experience valve failure. These enlarged vessels create the characteristic bulging appearance that concerns many individuals. Unlike spider veins, varicose veins can cause significant discomfort and may indicate underlying circulatory problems requiring medical evaluation.
This vascular breakdown process affects millions of people and understanding its mechanics helps explain why certain lifestyle factors can trigger sudden vein visibility.

Common Triggers And Contributing Factors
These lifestyle factors create conditions that either increase vein pressure or weaken vein walls, making previously hidden vessels suddenly visible. Physical activity and exercise can temporarily cause veins to bulge as increased blood flow and muscle contractions push more blood through the circulatory system. While this effect usually subsides after activity, intense or frequent exercise may contribute to long-term vein visibility.
Environmental and clothing factors play significant roles in sudden vein appearance. Sun exposure damages skin elasticity, making underlying veins more prominent through thinner skin. Hot temperatures cause blood vessels to dilate, increasing their visibility, while tight clothing around the waist and legs restricts proper circulation and creates pressure points that force blood to pool in affected areas.
Age represents the most unavoidable contributing factor, as time naturally weakens vein structures and valve function. This deterioration makes older adults increasingly susceptible to visible veins, with the process often accelerating after age 50. Hormonal fluctuations during pregnancy, menopause, or birth control use further compromise vein wall integrity, explaining why women experience these issues more frequently than men.
Prolonged standing or sitting creates sustained pressure within leg veins, restricting the natural muscle contractions that assist blood flow back to the heart. This static positioning allows blood to accumulate in lower extremities, gradually stretching vein walls. Being overweight compounds these issues by adding excess pressure on the entire venous system, particularly affecting leg circulation where gravity already challenges blood return.
These factors often work in combination, creating the perfect conditions for sudden vein visibility that concerns many individuals.

Recognizing Symptoms And Risk Assessment
When these contributing factors converge, they manifest through distinct symptoms that signal developing vein problems. Beyond simple visibility, varicose veins present characteristic sensations that differentiate them from harmless spider veins. Patients commonly experience aching and heaviness in affected areas, particularly after prolonged standing or sitting periods.
The legs may feel unusually tired or cramped, with symptoms typically worsening throughout the day and improving with elevation or rest. Swelling around the ankles and lower legs becomes increasingly noticeable, often accompanied by itching or skin irritation around the affected veins. The skin may develop discoloration ranging from brown to reddish patches, sometimes taking on a leathery texture that indicates advancing venous insufficiency.
Genetic predisposition significantly influences an individual’s likelihood of developing these symptoms. Family history plays a major role in determining vein wall integrity and valve deterioration patterns. Studies demonstrate that women face twice the risk of developing varicose veins compared to men, primarily due to hormonal fluctuations throughout different life stages.
Age remains the most decisive risk factor, with nearly 40% of women and 20% of men developing significant vein problems by age 50. Being overweight compounds these risks by creating additional pressure on leg veins, further restricting blood flow returning to the heart.
Understanding these symptoms and risk factors enables early recognition and appropriate response to potentially serious vein complications.

Medical Complications And When To Seek Help
These serious vein complications extend far beyond cosmetic concerns when left untreated. Chronic venous insufficiency develops when damaged veins cannot effectively return blood to the heart, causing persistent swelling and progressive skin changes that worsen over time.
Venous ulcers represent one of the most concerning complications, typically forming near the ankles where circulation is poorest. These open wounds heal slowly due to compromised blood flow and can become infected without proper medical intervention, requiring extensive wound care to prevent further deterioration.
Blood clots pose the greatest immediate threat to patient safety. Superficial thrombophlebitis affects surface veins, while deep vein thrombosis involves deeper vessels and can prove life-threatening. When blood clots travel to the lungs, they cause pulmonary embolism, a potentially fatal condition requiring emergency medical treatment.
Certain symptoms demand immediate medical attention. Sudden onset of severe leg pain, swelling, or unusual warmth may indicate deep vein thrombosis requiring urgent intervention. Bleeding from bulging veins, even minor episodes, warrants prompt medical evaluation to prevent serious complications.
Skin ulcers or wounds near affected veins need immediate professional assessment to prevent infection and promote proper healing. Changes in skin color or texture around bulging veins may signal advancing venous insufficiency that requires specialized treatment planning.
While prevention through regular exercise, weight management, and avoiding prolonged immobility helps reduce risks, recognizing these warning signs ensures timely medical intervention when complications arise.
Continue Reading →